- Floater Treatment
- Dry eye - Meibomian Gland dysfunction
- Age-Related Macular Degeneration (AMD)
- Diabetes and Eye Care
- Glaucoma Treatment
- Dry Eye - Lipiscan, Lipiflow
- Retinal Detachment
What is vitreolysis?
Also known as floater laser treatment, vitreolysis is a non-invasive, pain-free procedure that can eliminate the visual disturbance caused by floaters. The goal of vitreolysis is to achieve a “functional improvement”. That is, to allow you to return to “normal” day-to-day activities without the hindrance of floaters.
How does vitreolysis work?
Vitreolysis involves the application of nanosecond pulses of laser light to evaporate the vitreous opacities and to sever the vitreous strands. During this process, the floater’s collagen and hyaluronin molecules are converted into a gas. The end result is that the floater is removed and/or reduced to a size that no longer impedes vision.
What happens during the procedure?
Vitreolysis is performed as an outpatient procedure; you do not have to stay overnight in a hospital. Immediately prior to treatment, your ophthalmologist will administer eye drops to provide mild anesthesia. A contact lens will then be placed on your eye, with the laser light delivered through a specially designed microscope. During treatment, you will likely observe small, dark specks/shadows – signaling that the floaters are being evaporated into small gas bubbles. These gas bubbles quickly dissolve and reabsorb into the vitreous. Once the treatment is complete, your ophthalmologist may treat your eyes with anti-inflammatory drops. Each treatment session typically takes 20-60 minutes to perform and most patients will need to undergo two treatment sessions, sometimes three, in order to achieve a satisfactory result.
What can I expect after treatment?
You may observe small, dark specks in your lower field of vision immediately following treatment, but these small gas bubbles will quickly dissolve. It is also important to note that some patients may experience mild discomfort, redness or temporarily blurred vision directly following treatment.
Complications and side effects
Reported side effects and complications associated with vitreolysis are rare. Side effects may include cataract and intraocular pressure (IOP) spike.
Who will benefit from vitreolysis?
It is necessary to undergo an ophthalmic examination to determine your eligibility for vitreolysis treatment.
• Age. In most cases, younger patients (<45) suffer from microscopic floaters located close to the retina (1-2 mm) and are not considered to be good candidates for vitreolysis treatment.
• Onset of Symptoms: If your floater symptoms develop very quickly then they may be associated with PVD, which can be treated with vitreolysis.
• Floater Characteristics. Large floaters with a soft border, situated away from the retina, are ideally suited to treatment with vitreolysis
Types of Eye Floaters
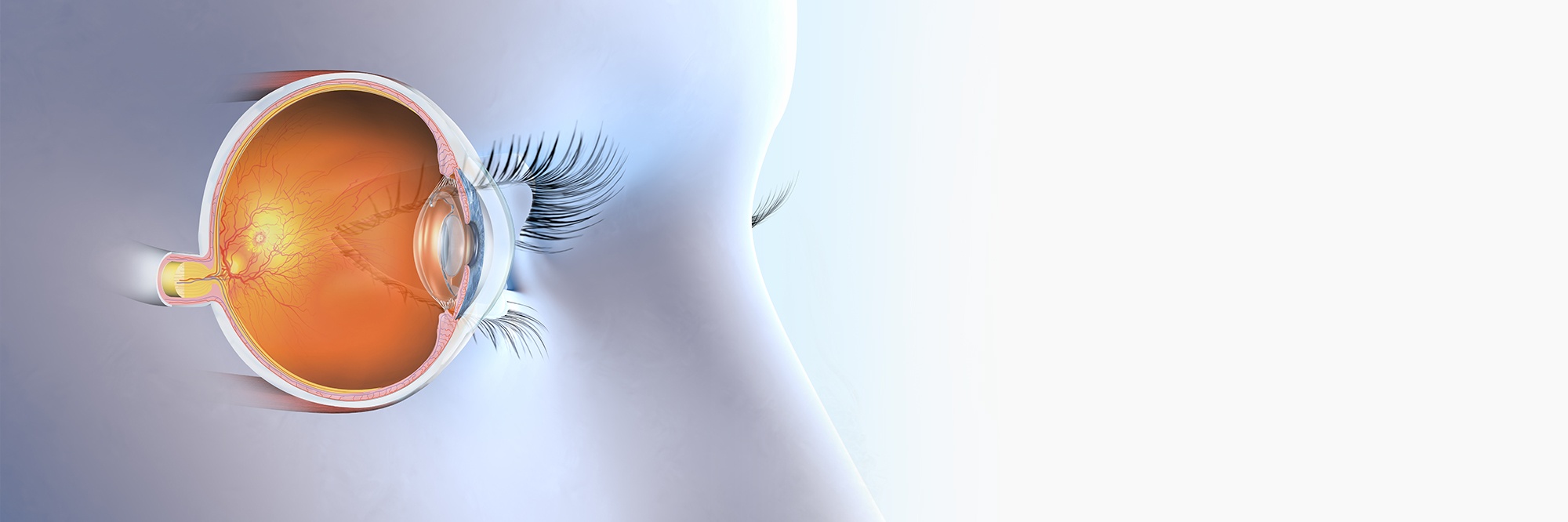
Eye floaters are small pieces of debris that float in the eye’s vitreous humor. This debris casts shadows onto the retina (the light-sensitive tissue layer at the back of the eye). If you have eye floaters, it is these shadows that you see “floating” across your field of vision.
Fibrous Strand Floater: Most common in young people, this thin, dense floater can appear as multiple dots and/or string-like cobwebs and is a result of clumping of the collagen fibers of the vitreous. Depending on size, and where it is located, it may be treatable with vitreolysis.

Diffuse Floater: This cloud-like floater is caused by the natural aging process. Whilst this type of floater can sometimes be treated with vitreolysis, it often requires more overall treatment in order to obtain satisfactory results.

Weiss Ring Floater: The ring-shaped Weiss Ring floater is a large, fibrous floater that is usually located safely away from the crystalline lens and the retina. Because of this, it can be treated safely and effectively with vitreolysis.

Meibomian gland dysfunction (MGD) is a common eye condition, yet many people don't realize they have it. You get it when there's a problem with a few dozen tiny glands in your eyelids that help make the oil layer of your tears. The most common type, obstructive MGD, happens when the gland openings get clogged, and less and less oil reaches the eye surface.
Lipiflow - What is Lipiflow? The Lipiflow procedure is a curative procedure where a device that produces heat and mild lid pressure is applied to the patient's eyelids (most patients state it feels like an eyelid massage), so that the blocked lipids will flow back normally into the tear fill.
Macular Degeneration is an age-related degenerative disease of the macula. The macula is a small area at the very centre of your retina which is responsible for fine, detailed central visual tasks such as reading. By damaging the macula, AMD can slowly take away your central vision. Unless detected in a routine eye exam, you may not even realize that you have the disease until it reaches an advanced stage.
How is AMD Diagnosed?
The best way to diagnose this disease is through routine eye exams with your retinal specialist. Dr. Patodia also offers specialized tests which determine if there are signs of AMD.
Intravenous Fluorescein Angiography (IVFA)
Fluorescein angiography is a diagnostic procedure which uses a special camera to take a series of photographs of the retina – the light sensitive tissue in the back of the eye.
A special water-soluble dye (fluorescein) is injected into a vein in the hand. The dye then travels through the veins and into the arteries, which circulate throughout the body.
As the dye passes through the blood vessels of the choroid and retina, the photographer takes a series of images in rapid succession. This allows the doctor to see signs of circulation problems, swelling, leakage, or abnormal blood vessel formation.
Heidelberg Spectral Domain Optical Coherence Tomography (Spectralis™ OCT)
The Spectralis™OCT is a laser imaging system which allows the doctor to see a 3-D image of the internal structure of the retina. This non-invasive test takes only a few minutes to preform, offering our patients the best, state of the art retina diagnostics in the world today.
Treatment
Lucentis™ Intravitreal Injection
Lucentis works by inhibiting the growth of the abnormal blood vessels that cause AMD. It is also used to treat swelling of the macula due to AMD. The goal of treatment is to prevent further loss of vision. Although some patients have regained vision, the medication may not restore vision that has already been lost.
Eylea® Intravitreal Injection
Eylea is used to treat wet age-related macular degeneration. It is also used to treat swelling in the retina caused by a blockage in the blood vessels. Eylea is also used to treat diabetic retinopathy, an eye disorder in diabetics that can lead to a buildup of fluid in the retina and cause blindness.
Can my eyes be affected by diabetes?
Patients with diabetes are more likely to develop eye problems such as cataracts and glaucoma, but the disease’s effect on the retina –specifically the blood vessels in the retina – is the main threat to vision. Diabetic retinal disease is the leading cause of blindness for people under the age of 65 in the developed world. Most patients develop diabetic changes in the retina within 7 years of being diagnosed with Type I diabetes. Most Type II diabetics have retinal damage when they are first diagnosed with diabetes.
Who is affected by Glaucoma?
How do I know if I have early signs of Glaucoma?
Early detection may prevent loss of vision. Using the HRT III, Dr. Patodia has one of the best diagnostic instruments available. It has been shown in hundreds of studies that 3-D measurement of the optic nerve head is far superior to conventional examination methods. It provides objective results of the disease years before any noticeable symptoms appear, such as loss of peripheral vision.
With regards to glaucoma treatment, the HRT III examination takes only a few minutes and is completely painless. Pupil dilation drops are required. A high-resolution laser camera takes a series of 3-D scans of the optic nerve and measures up to 28 million individual points per exam. A computer compiles and analyzes the information from the scans and produces a “baseline” image which Dr. Patodia can assess and compare with future exams. Over time, these scans allow Dr. Patodia to see even the smallest changes which help to detect and manage glaucoma.
What are some Glaucoma treatment options?
YAG P.I.
This procedure creates a microscopic hole in the coloured part of the eye, known as the iris. YAG Peripheral Iridotomy is an essentially painless procedure that takes only several minutes to perform.
Selective Laser Trabeculoplasty (SLT) Laser
Selective Laser Trabeculoplasty is a laser treatment to the natural internal drain of the eye. It is felt that the laser induces the body’s own natural healing processes to “clean out” the internal drain, thereby reducing pressure in the eye.
Medicated Drops
Trabeculectomy
Coming Soon
A small hole or tear in the retina left untreated runs the risk of retinal detachment. A retinal detachment is a peeling away of the retina from the wall of the eye with resulting loss of vision. Retinal detachment can be repaired and is usually quite successful. However, this can involve significant surgery and it is better if it can be prevented.

How is it treated?
This is treated with laser cryopexy pneumatic retinopexy or vitrectomy and scleralbuckle.
Retinal Cryopexy
Dr. Patodia uses a probe that is chilled to -80 degrees Celsius. After administering a small amount of local anaesthetic to the white, external surface of the eye, the probe is applied to the outside wall or white of the eye and a spot weld around the tear is fashioned to secure the tear in place. This prevents an enlargement of the tear or detachment of the retina in a vast majority of cases.
After treatment, patients will be given a prescription for antibiotic drops, to be used four times a day for four days.